Citing ‘pending legal challenge,’ Indiana suspends its Medicaid work requirements; lawsuit is fourth one to challenge them
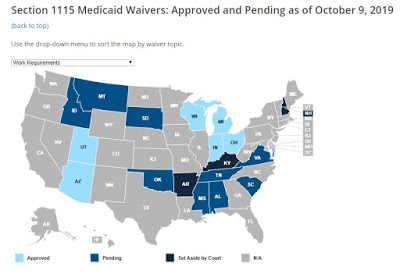
Kaiser Family Foundation graphic
—–
Indiana’s Medicaid program has temporarily suspended its work and community-engagement requirements “due to a pending legal challenge,” according to an Indiana state news release.
The lawsuit against Indiana is the fourth federal challenge to a state’s attempts to add work and community-engagement requirements to the Medicaid program, James Romoser reports for Inside Health Policy. The other three have been in Arkansas, Kentucky and New Hampshire. All four states are led by Republicans.
Kentucky, led by Gov. Matt Bevin, was the first state to be approved, but a federal judge in Washington, D.C. blocked its plan twice, and stopped a similar plan that had already taken effect in Arkansas. A three-judge appellate panel appeared skeptical of both plans in a hearing Oct. 11. The panel is expected to rule within a few months.
The same federal district judge who ruled on the Kentucky and Arkansas cases, and blocked the New Hampshire waiver in July, is the judge for the Indiana lawsuit, Romoser reports. Since, the Centers for Medicare and Medicaid Services and New Hampshire have appealed the ruling, which places it in the same appeals court that is considering the legality of the Arkansas and Kentucky cases, Romoser reports in a separate article.
Judge James Boasberg of Washington, D.C., has said the waivers are invalid because CMS failed to explain how work requirements would promote Medicaid’s goal of providing health coverage.
Indiana health officials said they remain committed to the state’s “Gateway to Work” program and are delaying work reporting requirements to allow time for the state’s lawsuit to be resolved and give time for similar legal challenges to work their way through the appeals process.
That said, the work requirements would not have applied to all of the Indiana Medicaid enrollees, Lisa Gillespie reports for Louisville’ WFPL. “Out of about 400,000 enrollees, 80,000 would have had to track their hours and risk losing coverage if they didn’t.” she writes. Before the Arkansas program was shut down, 18,000 people lost their Medicaid coverage because of non-compliance.
Dustin Pugel, a policy analyst with the Kentucky Center for Economic Policy, told Gillespie that Indiana may have suspended its program because it would be an “administrative nightmare” to do so because of a court ruling.
“They voluntarily suspended, I assume, thinking about what will be coming similarly for them that came to New Hampshire, Arkansas and Kentucky,” Pugel said. “I imagine they were doing it this way so that they could smooth out any administrative bumps that could come up from having to pull the plug quickly in response to a judge’s order.”
Arizona has also suspended its plan to add work requirements to its Medicaid program due to all of the legal uncertainty.
Medicaid work and community engagement requirements have been a key difference between Kentucky’s gubernatorial candidates as they fast approach election day on Nov. 5.
At an Oct. 15 debate, Attorney General Andy Beshear pledged to drop the plan if elected because “This is paperwork and it is intended to tear health care away from people.”
Bevin replied, “This isn’t about people being, having anything ripped away from them. What I propose is that people work and or volunteer and or go to school or be in training or take care of someone in exchange” for their benefits.
Bevin’s original proposal estimated that in five years, Kentucky’s Medicaid rolls would have 95,000 fewer people than without the plan, largely because of noncompliance. Academic health experts said in a friend-of-the-court brief that a more likely range was 175,000 to 297,500. Medicaid covers 1.4 million Kentuckians, around 450,000 of them under the expansion of the program to the working poor under the Patient Protection and Affordable Care Act.
Studies have indicated that most people in Kentucky who would be affected by the work rules are already meeting them. One study based on polling estimated that 97% were already meeting the requirements; another, based on claims data, indicated that 64% were.
So far, 18 states have asked for a waiver of the traditional Medicaid rules to allow such requirements, with six of the waivers approved, nine of them pending and three of them set aside by the court, including those in Kentucky, Arkansas and New Hampshire, according to the Kaiser Family Foundation.