Republican legislators question cabinet’s figures on managed-care payments and cost projections for Medicaid expansion
 |
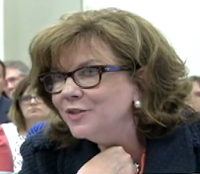
| Audrey Haynes (cn|2 image) |
“When
Audrey Haynes sat down before the legislature’s Medicaid Oversight and
Advisory Committee Wednesday, she expected the data she brought would
persuade lawmakers that Kentucky’s expansion of Medicaid has been good
for the state,” Ronnie Ellis reports for CNHI News Service. “The secretary of the Cabinet for Health and Family Services, which
administers the Medicaid program also may have expected her statistics
to ease unhappiness with the state’s move to managed care for most
Medicaid services.”
“It didn’t happen,” Ellis writes. “At least she didn’t persuade Republican members who openly questioned the validity of the cabinet’s data, a couple stopping just short of saying the cabinet is making up the numbers” about payments to providers by managed-care organizations, which it says are 99 percent on time. “The numbers do not appear to represent the reality on the ground,” Rep. Richard Benvenuti, R-Lexington, said after the meeting.
 |
| Sen. Ralph Alvarado |
“I think those are false,” Sen. Ralph Alvarado, R-Winchester, said after the meeting. “I don’t know if they’re lying, but somebody is providing bad information.”
During the meeting, Alvarado read “segments of letters from providers who have not received full reimbursements from managed care organizations,” reports Kevin Wheatley of cable channel cn|2‘s “Pure Politics.”
“Haynes referenced a report from CHFS which showed that over 90 percent of Medicaid claims are being paid in a timely manner,” reports the blog of the Kentucky Chamber of Commerce. “Sen. Alvarado replied that this statistic does not match what he is hearing from his constituents and medical providers.” Haynes addressed the managed-care issue in her PowerPoint presentation, downloadable here.
Rep. David Watkins, D-Henderson, a retired physician and co-chair of the committee, “urged the panel to find ways to improve managed care.”
Watkins said the managed-care organizations, which are insurance companies or their subsidiaries, should come before the committee to answer questions. “I’m not totally satisfied that they’re doing quite as good a job as your report here would portray,” he told Haynes. “I think they need to be more accountable. I think they need to be more responsive to the providers who actually are doing work in the field.”
The MCOs will appear before the joint House-Senate committee Aug. 19, Brad Bowman reports for The State Journal in Frankfort. For cn|2’s three-minute clip of the discussion between Haynes and Alvarado, via YouTube, click here.
The Republican lawmakers also voiced skepticism, but offered no contrary evidence, about the cost of expanding Medicaid to households with incomes up to 138 percent of the federal poverty level, from the previous limit of 69 percent. Under the Patient Protection and Affordable Care Act, the federal government is paying the entire cost of the expansion until next year, when the state will begin paying a small part, rising to the law’s cap of 10 percent in 2020.
Haynes noted projections for Democratic Gov. Steve Beshear’s administration that the expansion would add $30.1 billion to the state’s economy through 2021, and would pay for itself until then, even after the state starts picking up part of the cost. The numbers were not new; they were part of a study by Deloitte Consulting and the University of Louisville that Beshear released in February.
Republicans focused on the prediction that the expansion would cost the state a net $45 million in 2021. “I know that seems like a way long ways off and some of you may no longer
even be in the position to deal with it, but some of us probably will
and the taxpayers will,” said Alvarado, a physician.
Haynes “stated that she believed with the financial boost to the economy through jobs, the costs will be offset,” the blog of the Kentucky Chamber of Commerce reports.
“Now that we’re seeing the lowest unemployment that we’ve seen in our
state in quite a number of years, I’m sure each of you are amazed at how
that we’ve had all 120 counties in our state where the unemployment
rate has gone down,” Haynes said. “As this state continues to generate
revenue and hopefully, as is planned, this is a bridge program for
people who basically are hard-working people, but their employer does
not provide insurance or they have children and therefore that qualifies
them from an income basis for Medicaid.”