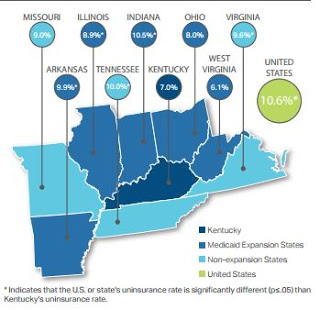
Share of Kentuckians without health coverage dropped to 7% in third quarter, lower than all neighboring states except W. Va.
 |
| Illustrations are from the report; click on images for larger versions |
An ongoing study of federal health reform’s impact in Kentucky has found that Medicaid expansion continues to help lower the number of Kentuckians without health coverage, which dropped to 7 percent in the third quarter of 2015. The uninsured rate was 9.8 percent in 2014, the first year of the expansion and federally subsidized health insurance. In 2013, it was 20.4 percent.
This rate is lower than the U.S. uninsured rate of 10.6 percent and “significantly lower” than four of the seven adjoining states plus Arkansas, said the Foundation for a Healthy Kentucky. The foundation is paying the State Health Access Data Assistance Center at the University of Minnesota more than $280,000 to study how the Patient Protection and Affordable Care Act is affecting Kentuckians. Data from this third-quarter report covers the July-September period.
Under health reform, then-Gov. Steve Beshear, a Democrat, allowed those with incomes up to 138 percent of the federal poverty level to enroll in Medicaid. Republican Gov. Matt Bevin’s administration is negotiating with federal officials for changes to the program that would make it less costly. The federal government is paying for the expansion through this year; next year states will start paying 5 percent, rising in annual steps to the law’s limit of 10 percent in 2020.
Bevin has said that Kentucky can’t afford to pay for the expansion. During his Jan. 26 budget speech said of the negotiations with federal officials, “If we cannot get it done we will not have the ability to have expanded Medicaid in the state of Kentucky.”
One of the essential health benefits of the reform law is free preventive health care, a benefit that thousands of newly insured Kentuckians have used.
The study found that during from July to September, Medicaid funded 1,180 diabetes screenings; 9,806 breast cancer screenings; 6,227 colon cancer screenings, with 5,561 of those for Medicaid expansion participants; and 82,056 dental services. In addition, Medicaid paid for 7,797 deliveries.
Treatment for substance abuse increased to 7,993 people during this quarter, up from 6,660 in the last quarter. The total included 5,758 Medicaid expansion participants.

This year, Kentuckians shopping for health insurance had more plans than ever to choose from on the state’s online health insurance marketplace, Kynect. The report noted that the exchange offered 60 plans in the enrollment period that ended Jan. 31, compared to 40 the year before.
And compared to Kentucky’s neighboring states, the study found that Kynect had the lowest median premiums for the “silver” level plan at $585.01. This was based on premiums for a 30-year-old couple with two children.
Bevin says he will abolish Kynect and have Kentuckians use the federal exchange; it remains to be seen whether insurers will put as many, more or fewer Kentucky plans on that exchange.
The study found that Medicaid enrollment remains concentrated in Eastern Kentucky, with 31 percent of the total; followed by Western Kentucky with 26 percent.