Study shows uninsured rate keeps falling, preventive services are popular and rural hospitals have more uncompensated care
Kentucky Health News
The share of Kentuckians without health insurance continues to drop, and new Medicaid enrollees continue to take advantage of free preventive health services, according to an ongoing study of federal health reform’s impact in the state.
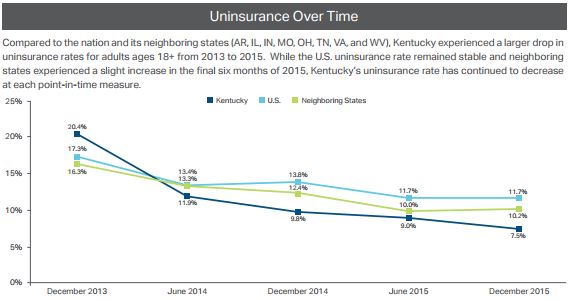
The report found that the rate of people without health insurance in Kentucky continues to drop.
In December 2015, the uninsured rate was 7.5 percent, down from 9 percent in June 2015. The national rate in December was 11.7 percent. In 2013, before the implementation of the PPACA, Kentucky’s uninsured rate was 20.4 percent.
Since December 2013, Kentucky’s uninsured rate has dropped 12.9 percentage points, more than double the national decline of 5.6 percentage points, says the report. Uninsurance rates can vary depending on how they are measured. This study used data from the Gallup-Healthways Well-Being Index, which produces state-level estimates of coverage twice a year.
“Lack of insurance is a significant barrier to getting necessary health care and preventive services timely,” Susan Zepeda, CEO of the Foundation for a Healthy Kentucky, said in a news release. “Tracking this and other key information about access to and cost of care in Kentucky helps to inform health policy decisions.”
Kentucky also continues to have a lower uninsured rate than its eight nearest surrounding states, although Ohio (7.6 percent) and West Virginia (7.7 percent) are catching up. Missouri (11.6 percent), Tennessee (13 percent) and Virginia (12.6 percent), the three states surrounding Kentucky that did not expand Medicaid, have the highest uninsured rates. (SHADAC map)
And while the state saw a smaller share of new health-insurance customers than the country overall (20 percent versus 39 percent), Kentucky had the largest percentage of re-enrollees (59 percent) return to Kynect, the state’s health insurance marketplace, to select plans compared to the rest of the nation (36 percent). Twenty-two percent of Kentuckians were automatically re-enrolled in plans.
Kynect, created by the Democratic administration of Steve Beshear, is in the process of being dismantled by the administration of Republican Gov. Matt Bevin, so Kentuckians will have to sign up for their health insurance through the federal exchange, healthcare.gov, during the next enrollment period which begins Nov. 1, 2016 and runs through Jan. 31, 2017.
Traditional Medicaid enrollees will sign up through Benefind, the state’s new one-stop-shop website that can be used to apply for Medicaid, the Kentucky Children’s Health Insurance Program (KCHIP), the Supplemental Nutrition Assistance Program (SNAP, once known as food stamps) and Kentucky Transitional Assistance Program (KTAP).
Expansion of Medicaid added about 400,000 Kentuckians to the program, and many of them have taken advantage of its free services to get screened for diseases and have physical or dental examinations.
 |
| Dark blue: traditional Medicaid enrollees Light blue: Medicaid expansion enrollees |
The latest report, which covers the fourth quarter of 2015, says 823 traditional Medicaid enrollees got screened for diabetes, compared to 2,959 Medicaid expansion enrollees. This was also true for colorectal screenings (see graph).
Overall, the study found that Medicaid covered 41,493 dental preventive services, 9,708 breast cancer screenings, 8,276 substance-abuse treatment services, and 5,589 colorectal-cancer screenings to enrollees aged 19-64.
Under federal health reform, Beshear expanded Medicaid to include those with incomes up to 138 percent of the federal poverty level. The federal government pays for this expanded population through this year, but next year the state will be responsible for 5 percent of the expansion, rising in annual steps to the reform law’s limit of 10 percent in 2020.
However, the future of the expansion is uncertain. Bevin has said that the state cannot afford its Medicaid population of about 1.3 million, and has charged his administration with designing a new Medicaid program, which will require federal government approval. He told reporters in early May that he was optimistic that the Centers for Medicare and Medicaid Services will approve the state’s new plan, but if they don’t it will be because “CMS does not want to see expanded Medicaid continue in Kentucky.”
The study found that Medicaid enrollment continues to be the highest in Eastern Kentucky with 31 percent participation, followed by Western Kentucky at 26 percent participation.
It also notes that while levels of uncompensated care have dropped for both urban and rural hospitals since 2013, rural hospitals saw slight increases in uncompensated care in 2015. (SHADAC graphic)
For the full report, click here.


