Average premiums on most popular Obamacare plan in U.S. will drop 1.5% in 2019; go up 9% in Ky.; state still lower than average
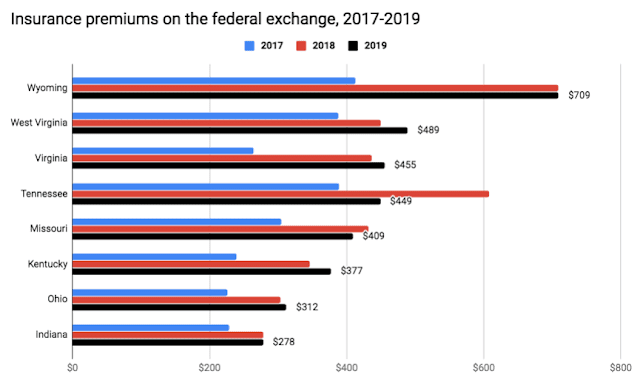
Chart from Insider Louisville
—
The average premium for the most popular health insurance policy on the federal exchange, called the “silver plan,” will drop by 1.5 percent next year — but not in Kentucky, where the rate for that same plan will increase by 9 percent.
A Centers for Medicare and Medicaid Services news release notes that 2019 will be the first year the national average has dropped since full implementation of the Patient Protection and Affordable Care Act in 2014. This year the average premium for these benchmark “Obamacare” plans increased by an average of 37 percent, and by 25 percent the prior year.
Nationally, CMS says a 27-year-old, single non-smoker who gets insurance through the exchange, HealthCare.gov, will pay an average annual premium of $4,872, down from $4,944. In Kentucky, that will rise to $4,524, from $4,152.
Healthcare.gov customers in 17 of the 39 states will see declines, three will see no change and customers in Kentucky and 19 other states will see an increase in their premiums in 2019, Boris Ladwig reports for Insider Louisville.
Ladwig adds that despite the 9 percent increase in Kentucky, the state’s rates for 2019 remain in the lowest third among the 39 state in the exchange. In Kentucky, about 90,000 people signed up for an Obamacare plan during the 2018 open enrollment. Nationally, that number was around 12 million.
CMS has said the reduction is a result of the Trump administration’s efforts to stabilize the individual market, but the Kaiser Family Foundation, and other health experts, say it is a result of insurers overcompensating their rates in 2018 after the administration lowered the subsidies it paid to insurers and also because insurance companies that offer Obamacare plans are making a profit.
In Kentucky, Anthem Health Plans of Kentucky and CareSource will offer federally subsidized plans on Healthcare.gov, with rate increases of 4.3 percent and 19.4 percent, respectively. Anthem will expand its coverage area into 34 counties it once served, to cover a total of 93. CareSource will cover 61 of the state’s 120 counties.
The Kentucky market president for CareSource, Michael Tayler, told Kentucky Health News in an e-mail that its premium increases for 2019 result from a number of factors.
“The elimination of the individual mandate that relieved the consumer tax penalty, and inflation related to medical and prescription drug costs, both impacted our rate decisions,” he said. “It’s these factors and other federal policy changes related to short-term limited duration and association plans that will most likely cause consumers with the greatest health care needs to enroll. These changes may create a gap in marketplace participation and ultimately a greater risk for insurers.”
The Kentucky Department of Insurance and Anthem did not respond to requests for comment.
Open enrollment on HealthCare.gov begins Nov. 1 and will run through Dec. 15.