Study: Private insurance pays hospitals 241% more than Medicare (186% in Kentucky); suggests shift to a Medicare model
By Melissa Patrick
Kentucky Health News
As health-care costs continue to rise for both employers and employees, one group of researchers says private insurers should move away from how they pay for hospital services, which requires them to pay a percentage of billed charges, and start paying the way Medicare does, based on a fixed-price agreements that are transparent to all. The American Hospital Associationsays that would not be sustainable, because Medicare doesn’t pay hospitals enough.
The Rand Corp., a global research firm, made this recommendation based on its a study that found private health plans in the U.S. paid hospitals 241 percent more than what Medicare would have paid them in 2017, up from 236% in 2015.
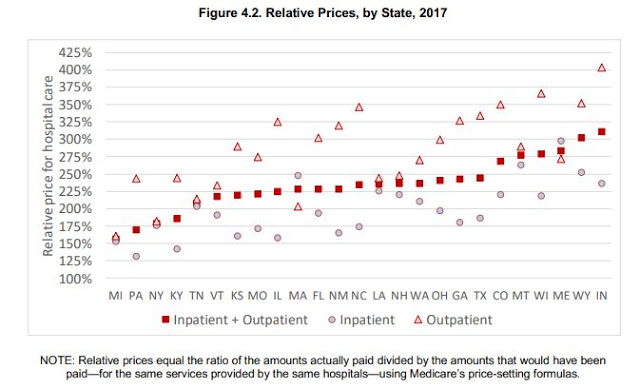
Kentucky’s private plans paid 186% more than Medicare in 2017, the fourth smallest difference among those in the 25 states surveyed. For inpatient treatment, the state’s costs were second lowest of the 25, but its outpatient costs were above average.
All but five Kentucky hospitals in the study had a rate greater than 200% of what Medicare pays for outpatient services, with nearly 19 greater than 300% for that same measure. There was a bigger difference in prices for outpatient care than for inpatient care. In Kentucky those rates were 245% and 142%, respectively; nationally, they were 293% and 204%.
“The widely varying prices among hospitals suggests that employers have opportunities to redesign their health plans to better align hospital prices with the value of care provided,” Chapin White, the study’s lead author and a policy researcher at Rand, said in a news release. “Employers can exert pressure on their health plans and hospitals to shift from current pricing system to one that is based on a multiple of Medicare or another similar benchmark.”
The report says the data is also important because it allows employers to create networks that move their employees away from the higher-priced hospitals to the lower-priced ones.
The study reported on the relative price of private insurance to Medicare by dividing the amount allowed for private insurance by the amount allowed for Medicare for the same service, in the same facility. The researchers used data from about 4 million patients in 1,589 hospitals in 25 states.
The researchers used claims data from self-insured employers, two state all payer claims databases and records from health insurance plans that chose to participate. For each private claim, they re-priced the service using Medicare’s grouping and pricing formulas.
Prices varied greatly by state and hospital. Of the 36 Kentucky hospitals in the study, private health-plan prices for outpatient services ranged from 85% of Medicare at Jane Todd Crawford Hospital in Greensburg to 526% at TJ Samson Community Hospital in Glasgow.
The study looked at three Kentucky hospital systems, including Baptist Health, Catholic Health Initiatives and Norton Healthcare. It found a decrease in relative pricing in each of the systems since 2015, with Baptist Health billing private insurers 168% more than Medicare in 2017, down from 203% in 2015; CHI billing 187% more in 2017, compared to 236% in 2015; and Norton Healthcare billing 185% more in 2017, compared to 205% in 2015.
Overall, the study found a wide variance among hospital systems, ranging from 150% of Medicare rates at the low end and more than 400% at the high end. “In general,” the report says, “prices paid by private health plans are much higher than Medicare, and there is a wide variation.”
The researchers found that if employers and health plans participating in the study reduced their hospital payments to Medicare rates, it would have resulted in $7.7 billion in savings for employers in 2015-17. It said reducing prices from the 75th to the 25th percentile would have reduced employer spending by $1.4 billion, about 40% of the employers’ and plans’ spending on hospitals in 2017.
The analysts offered two different interpretations for this variation. One is the “cost shifting story,” which argues that Medicare severely underpays hospitals, compelling them to charge privately insured patients more. The other is “the leverage story,” which says hospitals have used their leveraging power to extract unreasonable price deals from health plans, which in turn makes Medicare prices “look woefully inadequate by comparison.”
The challenge is that while employers are looking for ways to decrease health-care costs, hospitals depend on cash flow generated by private insurance plans to upgrade and expand their services. “Lower private prices would require hospital managers to find ways to increase revenues to reduce costs to maintain current margins,” says the report.
The American Hospital Association released a statement that took issue with the small sample size, which it described as less than 5% of all covered persons in about half of all states, and just 2% of the 181 million Americans with employer-sponsored insurance nationally.
It also took issue with the usage of Medicare payment rates as the benchmark for hospital prices, stating that in 2017, hospitals received payment for only 87 cents for every dollar they spent caring for Medicare patients.
“Simply shifting to prices based on artificially low Medicare payment rates would strip vital resources from already strapped communities, seriously impeding access to care,” AHA General Counsel Melinda Hatton said. “Hospitals would not have the resources needed to keep our doors open, innovate to adapt to a rapidly changing field and maintain the services communities need and expect.”
All that said, many think something has to give. Employers have increasingly shifted to high-deductible plans to help offset some of their costs, but this has created a situation where employees have become “under-insured” because they can’t afford the cost burden that comes with such plans.
Further, according to an analysis by The Commonwealth Fund, the cost of employer health-insurance premiums and deductibles continues to outpace wages. The analysis found that Kentucky families covered through work spent, on average, 13% of their income for health coverage in 2017.
The study recognizes that it only used data for about one-third of U.S. hospitals, and that for many of those hospitals, only outpatient prices could be reported; and that it only includes facility claims and not claims for treatment by physicians or claims for prescription drugs.
The report offers detailed suggestions on how employers can use this data to seek lower prices for their health plans. It also includes suggestions for policymakers, including placing limits on payments for out-of-network hospital care or allowing employers to buy into Medicare or another public option that pays providers based on a multiple of Medicare rates.
The research was funded by the Robert Wood Johnson Foundation, the National Institute for Health Care Reform, and the Health Foundation of Greater Indianapolis and participating self-insured employers.