Plan to change how some rural hospitals are paid would hike pay to 39 in Ky., totaling $4 million a year, hospital association says
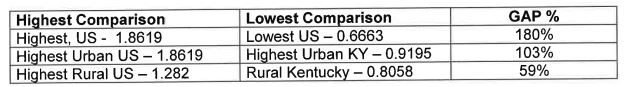
Table from Kentucky Hospital Association letter endorsing changes in the Medicare wage index.
—–
By Melissa Patrick
Kentucky Health News
A Trump administration plan to change the way Medicare pays hospitals, and perhaps keep some rural hospitals from closing, would give some rural Kentucky hospitals a financial boost.
A proposed rule would raise reimbursement rates, starting in October, for rural hospitals paid under the “inpatient prospective payment system” by reducing payment to the nation’s better-off hospitals.
The Kentucky Hospital Association is in full support of the proposal, it said in a May 30 letter to the Centers for Medicare and Medicaid Services (CMS).
“Every Kentucky rural hospital paid under the inpatient prospective payment system would be helped. It would increase payments to those hospitals by $4 million a year,” KHA President Nancy Galvagni told Kentucky Health News in an e-mail. “No payments to Kentucky urban hospitals would be cut. It is the high-cost hospitals in the Pacific and New England states whose payments would be lowered.”
KHA says 39 of the state’s rural hospitals would benefit from this new payment model. The state has 127 hospitals.
Some critics of the plan note that it doesn’t apply to critical-access hospitals, which comprise about half the rural hospitals in the country. Kentucky has 27 such hospitals, which are generally in rural areas and have 25 or fewer beds.
Currently, Medicare reimbursement rates for hospitals in the inpatient prospective payment system are calculated by first determining a base payment for each patient, based on their diagnosis and the severity of their illness. It then factors in a wage index for the labor-related share of the costs.
The index is based on how much a hospital pays its staff, so hospitals in areas with high living costs get higher reimbursements than areas that have low cost of living — for the same services.
The wage index has shortchanged Kentucky hospitals; the proposed 2020 index ranks Kentucky 36th in rural wages, “and no rural or urban area in Kentucky has a wage index at or above 1.0,” the lowest ranking in the index, the hospital association said in its letter to CMS.
A labor market’s wage index is the ratio of its average hourly wage to the national average hourly wage, according to CMS.
KHA says the wage-index disparities mean Kentucky’s rural hospitals get approximately 26 percent less — $1,800 per case — than the state with the highest rural wage index. Kentucky’s urban hospitals with the highest wage index get 40 percent less, $3,700 per case, than hospitals with the highest urban wage index “for providing the exact same level of care to Medicare beneficiaries,” KHA says.
The lobbying group points out, “The wage index is a significant issue for Kentucky’s hospitals because Medicare covers about one-half of all patients treated in hospitals.”
The proposed rule would reduce the disparity in reimbursements by increasing the wage index for hospitals in the bottom fourth of payments and reducing the index of those in the top fourth, creating a budget-neutral shift of funds, a CMS news release said.
“This policy change is needed to improve the fairness of Medicare payments necessary to protect access to care for every American,” KHA said in its letter.
But not everyone supports the proposal.
The American Hospital Association said in a letter to CMS that while it supports increasing the wage index for low-wage hospitals, “this should not be accomplished by penalizing other hospitals,” especially because Medicare reimburses most hospitals “below the cost of care.” It adds that there is no legal requirement for the adjustment to be budget-neutral.
The Office of Inspector General in the Department for Health and Human Services called for a complete overhaul of the system after it conducted a studythat found, among other things, that the wage index often relies on inaccurate wage data and CMS lacks authority to penalize hospitals that submit inaccurate or incomplete data. The report estimated a total of $140.5 million in over-payments to 272 hospitals resulted from the inaccurate data between 2004 and 2017.