Preliminary estimates of covid-19’s effects on health-care system, and lives, show Ky. compares favorably with major border states
These estimates, based on data through March 24, are being revised daily, as noted below.
—–
By Al Cross
Kentucky Health News
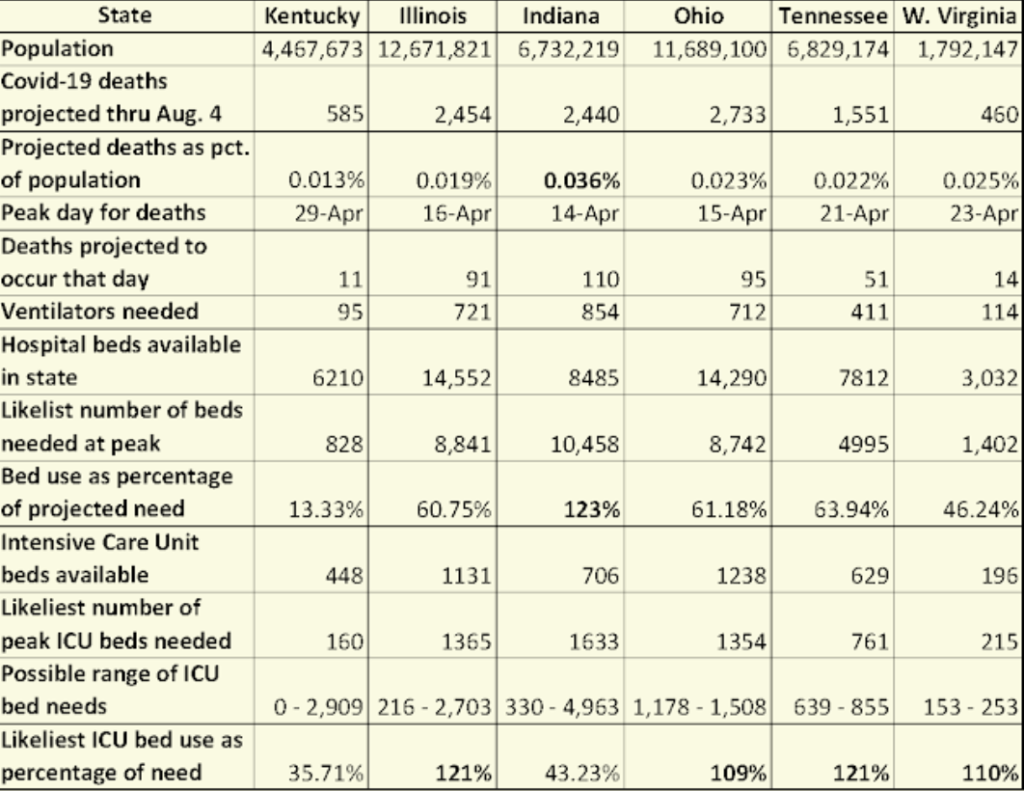
Kentucky compares favorably to its major bordering states in the first public estimates of the impact of the coronavirus on the U.S. health-care system and the number of deaths expected from the covid-19 disease caused by the virus.
However, some estimates for Kentucky have wider possible ranges than for the other states, illustrating the shortage of data that public-health experts say is needed for policymakers to make decisions.
The estimates were published Thursday by Christopher Murray, director of the Institute for Health Metrics and Evaluation at the University of Washington. It drew in confirmed covid-19 deaths around the world through March 24, and state-by-state data on hospital capacity and use. He said he used covid-19 data “from select locations to develop a statistical model forecasting deaths and hospital utilization against capacity by state for the U.S. over the next four months.”
Murray plans to update his report daily. “Every day that we get more data, we’ll get better predictions,” he told The Washington Post. “We believe the data on deaths, but we don’t believe the data on number of cases basically almost anywhere because of variability in testing protocols.”
Murray estimated that 585 people in Kentucky will die from covid-19, or 0.013 percent of the state’s estimated 2019 population. That is lower than any of the states that have major borders with Kentucky. Indiana’s percentage is the highest, 0.036%, representing a forecast of 2,440 deaths.
The death forecasts for other major adjoining states are: Illinois, 2,454 (0.019%); Ohio, 2,733 (0.023%); Tennessee, 1,551 (0.022%) and West Virginia, 460 (0.025%).
Deaths in a pandemic typically follow a bell-shaped curve. Murray estimated the peak of the curve for each state and the likeliest number of deaths on that day. Of the six states, Kentucky has the latest forecast peak date, April 29May 11, when 11 people are projected to die. Indiana is forecast to have the earliest peak among the six, 11034 deaths on April 1714.
Projections above for Kentucky, below for Tennessee; shaded areas indicate possible ranges.
To view a larger version of either image, click on it. Images have been squeezed horizontally.

Health experts talk of the need to “flatten the curve” to keep the number of cases from overwhelming the health-care system, and Kentucky appears to be doing that. Murray estimated that the state will have enough hospital beds for covid-19 patients, but his forecast is less certain when it comes to the number of intensive-care-unit beds.
His report estimates that most of the major border states will be short of ICU beds at the peak, but Kentucky probably will have enough: 448 when only 160 are likely to be needed. However, the report says the number needed could be as low as zero or as high as 2,909.
The wide possible range could stem from the relatively low number of cases and deaths reported in Kentucky through March 24.
Gov. Andy Beshear was asked at his Sunday press conference if he had a projected peak date for Kentucky. “We’re working on that,” he said. “It’s all based on some really limited data. … The next two weeks are critical, and we know that will impact the peak.”
Kentucky Health News notified Beshear’s office before the press conference that it was preparing a story on the report, offering him a chance to comment on it. He did not, at least directly.
Beshear and Health Commissioner Steven Stack said the critical measure in the next two weeks is social distancing to prevent spread of the virus. “We’re at crunch time,” Stack said. “Assume everybody around you has the coronavirus.”
One major obstacle to dealing with the virus is the lack of testing, which could track its spread. widespread testing would identify people who have the virus but no symptoms, Dr. Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases, said on CNN. People without symptoms can still spread the virus, and not develop symptoms until two weeks or more after becoming infected.
The University of Washington model presumes that federal guidelines for social distancing will stay in effect through May. “That’s what we believe is going to happen because nobody’s really going to want to let up,” Murray told The Washington Post. “Even if the deaths are trending down nationally, some states may still be going up.”
Murray’s report estimated that as many as 162,000 Americans will die from covid-19, but that the number could be as low as 38,000. It said the likeliest number is 81,114 deaths.

“In addition to a large number of deaths from covid-19, the epidemic in the U.S. will place a load well beyond the current capacity of hospitals to manage, especially for ICU care,” Murray wrote.
Murray’s results closely resemble those from a model developed by federal scientists, said Deborah Birx, coordinator of the White House’s coronavirus task force. “When we finished, the other group that was working in parallel, which we didn’t know about, IHME and Chris Murray, ended up at the same numbers,” Birx said at President Trump’s daily press conference Sunday.
Among the states bordering Kentucky, Indiana is the only one that Murray’s report forecasts to be short of beds, but only it and Kentucky are predicted to have enough ICU beds.
“The estimated excess demand on hospital systems is predicated on the enactment of social distancing measures in all states that have not done so already within the next week,” Murray wrote, “and maintenance of these measures throughout the epidemic, emphasizing the importance of implementing, enforcing, and maintaining these measures to mitigate hospital system overload and prevent deaths.”