Pandemic still set records but may be nearing its crest in Ky.; short-staffed hospitals struggle to keep up; better masks urged
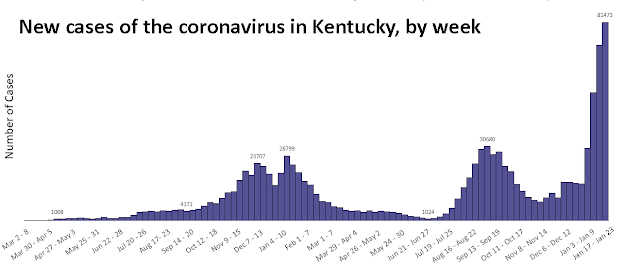
State Dept. for Public Health graph, adapted by Ky. Health News; for a larger version, click on it.
—–
By Melissa Patrick
Kentucky Health News
As hope mounts that the Omicron-variant surge will soon crest in Kentucky, hospitals in the state remain strained with a workforce that is struggling to stay healthy, prompting Health Commissioner Steven Stack to say the state is not running out of beds and ventilators, “We’re running out of health-care workers.”
Kentucky has averaged 11,489 new cases of the coronavirus in the last seven days, less than the seven-day average reported last Friday, and lower than the record high seven-day average of 11,789 set Sunday.
Another sign that the surge may be cresting is a four-day decline in the daily infection rate, now 216 daily cases per 100,000 residents. On Friday it was 237.01, the highest ever.
Sixty-six of the state’s 120 counties have above 200. The lowest rate, 62.7, is in Elliott County. The New York Times ranks Kentucky’s rate 16th among the states.
In the reporting week ended Sunday, the state hit another case record and positive-test rate. It had 82,159 cases, more than 9,000 above the previous record-setting week, and a positivity rate of 33.1%, nearly four percentage points higher than the record set the previous week.
On Monday, the share of Kentuckians testing positive in the past seven days was 33.06%, meaning that one in three Kentuckians who get tested for the virus are positive. The number does not include at-home tests.
Offering a bit of hope, Stack said if Kentucky follows the case trends in Rhode Island, New York and the United Kingdom, Kentucky should reach its peak number of cases this week or next.
Gov. Andy Beshear said, “We hope that we are cresting, that we are near the peak of what we’ll see. Remember, even if that’s the case, it’s going to take us at least a couple of weeks if not three to get to a much safer place.”
He said the virus is not hitting the lungs nearly as hard as it did as the other variants, but is infecting more people, including hospital workers.
Dr. Mark Dougherty, an infectious disease doctor at Baptist Health Lexington, said the same at a news conference with doctors from CHI Saint Joseph Health and UK HealthCare.
On Monday, Kentucky hospitals reported 2,326 Covid-19 patients, with 440 in intensive care and 257 on mechanical ventilation. Nine of the state’s 10 hospital regions were using at least 80% of their intensive care unit capacity, with three above 90%.
 |
| Cabinet for Health and Family Services graph, adapted by Ky. Health News; click on it to enlarge. |
Beshear held his weekly pandemic press conference remotely, announcing that his son, Will, 12, had tested positive for the coronavirus and is generally asymptomatic. He said Will is fully vaccinated and had received a booster shot, that he and the rest of his family had tested negative, that he would get tested daily, and that he would follow federal guidelines.
“As a parent, I never wanted . . . either of my kids to get Covid,” he said. “But I got them vaccinated to ensure that they were protected if they did.”
Stack said, “If you’re a parent who has not yet had your sons and daughters vaccinated, please talk to your pediatrician, your primary care provider, ask them about the vaccines. The American Academy of Pediatrics, numerous other medical associations, and other public health bodies have all recommended vaccination. It’s the safest way to keep kids healthy and well and in school and also to help protect their families at home who may be more vulnerable.”
Stack also noted that the vaccine helps to reduce the risk of the multi-system inflammatory disease that sometimes strikes children a couple of months after the initial infection, and sometimes puts them in intensive care.
At the hospitals’ news conference, Dr. Lindsay Ragsdale, interim chief medical officer at Kentucky Children’s Hospital, said the Covid-19 vaccine is 91% effective at preventing this inflammatory disease, called MIS-C, in children.
She also said the Children’s Hospital, part of UK HealthCare, is seeing an uptick in Covid-19 hospitalizations. Today, it was reported that there are six pediatric Covid-19 patients.
Ragsdale strongly encouraged parents to get their children vaccinated, noting that she is worried because there has been a drop in the number of children getting vaccinated at their vaccine clinic.
Only 50% of 16- and 17-year-olds, 47% of 12-to-15-year-olds, and 20% of 5-to-11-year-olds in Kentucky have received at least one dose of a vaccine.
Another key message at the hospitals’ news conference was that it’s time to step up the quality of the masks we are wearing, to either a KN95 or an N95.
Dougherty said about 40% of Baptist Health Lexington’s Covid-19 patients are admitted to the hospital for other reasons, which shows how prevalent the virus is in the community.
“It’s ubiquitous. It’s everywhere. It’s hyper-contagious,” Dougherty said. “And because of that, I think we need to step up the quality of masks that we’re using,” he said, adding that the advice applies both in and out of the hospital.
Ragsdale said KN95 masks for children are available, and encouraged parents to switch to them.
“It’s probably the best masks that we can offer for kids,” she said. “The cloth mask is better than nothing, but it’s really not as good as a KN95 to prevent spread for pediatric patients. . . . For schools, this would be a great addition as well to preventing spread,” she said.
Beshear was asked if the state was talking about supplying such masks to schools. He didn’t answer directly, but said the state provides about $100 million in testing assistance and surgical or near-surgical level masks through the Covering for Kids program, but not KN95s.
Stack’s advice was to “wear the best quality mask you can get that’s well fitting as reliably as you possibly can — so do the best you can with the best you have.” He noted that the federal government will be shipping KN95 masks to pharmacies and states, and they will need to figure out how best to deploy those.
“But I agree with the governor,” Stack said. “The first step is to require masks of any sort in the school setting, the next step then is to upgrade your masks. So I would be really grateful if we just got every student wearing masks to keep them in school safely.” Beshear noted that some schools aren’t requiring masks.
Stack said 23 of the deaths were in people 61 or younger, including one 20-year-old. Beshear Stack said he draws attention to these deaths because 94% to 95% of all the Covid deaths in Kentucky since July 1 have been in unvaccinated persons.
“Unfortunately, these sufferings usually don’t need to occur,” he said. “Vaccination almost entirely eliminates this risk. So I do hope more folks will continue to get vaccinated and protect themselves from that horrible outcome.”