By Melissa Patrick
Kentucky Health News
Kentuckians on Medicaid need to pay attention to any correspondence from the state’s Medicaid program. The Department for Medicaid Services has resumed its annual renewal process for Medicaid members because the pandemic rules that allowed continuous enrollment have ended.
The process that allows Medicaid agencies to restart the annual renewals — and kick off those who no longer qualify — has been dubbed “Medicaid unwinding,” a process that will take 12 months to complete, since it will use each Medicaid member’s renewal month.
“We are currently outreaching to individuals with a May 31 renewal date. This means those individuals have until that date to renew with Medicaid,” Susan Dunlap, spokeswoman for the Cabinet for Health and Family Services, said in an email.
“The most important thing Kentuckians on Medicaid need to be doing right now relating to the unwinding includes making sure we have up-to-date contact information,” Dunlap said. “That way, Medicaid can contact members about renewing, if needed. We are telling all our members to visit their account at kynect.ky.gov to review their information and make sure everything is correct. If they do not have an account, we recommend they create one.”
At a monthly stakeholder meeting in April, Deputy Medicaid Commissioner Veronica Judy-Cecil encouraged Kentuckians to use their Kynect health-benefits account for renewal. “It is going to be the fastest and easiest way for redetermination to be processed,” she said.
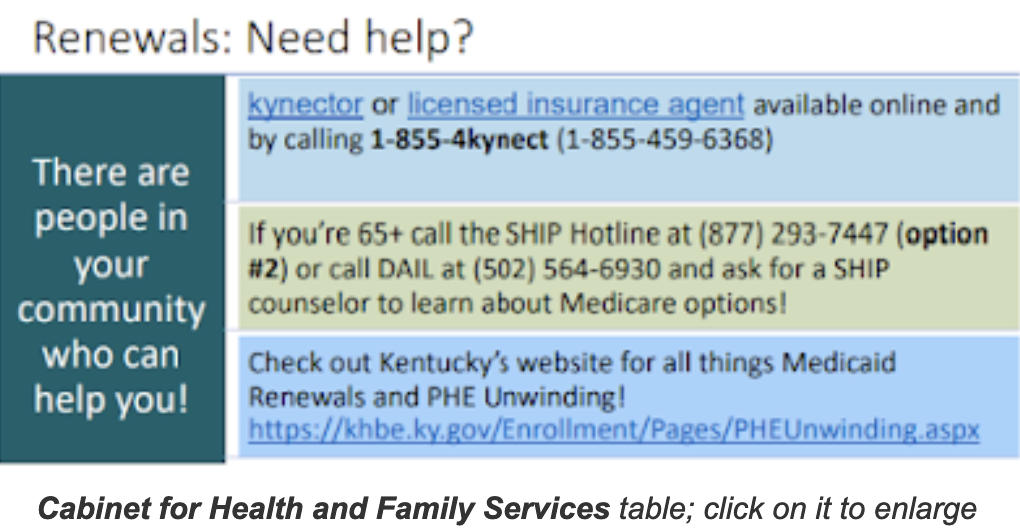
If not signed up for Kynect, Medicaid members can complete and return forms via mail or fax, Judy-Cecil said. They can also call Kynect (1-855-459-6328) or the Department for Community-Based Services, or visit a DCBS office, a licensed insurance agent, or a Kynector, who helps Kentuckians enroll in coverage through Kynect.
As the Medicaid rolls have piled up with automatic renewals and additional enrollments, a record number of Kentuckians were enrolled in the program on April 1: 1,725,467. But on that day, the state could resume removing people from the program, and enrollment for May declined to 1,712,381. (For county-by-county enrollment numbers, click here.)
In April, the Medicaid department “estimated approximately 240,000 may lose eligibility” in the unwinding, health-cabinet spokesman Brice Mitchell said in an email. “However, until someone goes through redetermination, it is impossible to accurately forecast who will lose eligibility.”
Of that 240,000, an estimated 75,000 have incomes over 138% of the federal poverty level, the Medicaid limit, and are likely to qualify for federally subsidized health insurance through Kynect.
Judy-Cecil said the state will reach out to Medicaid members about 90 days before their Medicaid renewal end date. Members will also get a notice about 60 days before their renewal end date and if there is no response by the 15th of their renewal month, they will get another notice. Members will get a renewal packet or a request for more information.
As of May 9, about 69,000 outreach calls had been made and over 17,791 calls had been received related to renewals, accoridng to the Public Health Emergency Unwinding website.
Judy-Cecil said Medicaid has prioritized contacting the Medicare-eligible population, since many Kentuckians stayed on Medicaid when they turned 65 instead of switching to Medicare. That’s because the national public-health emergency rules required the state to continue coverage to get extra federal funds.
The priority from July until the end of the unwinding will be to reach out to those on Medicaid who make too much money to stay on the program. Judy-Cecil said it’s important to make sure this group is aware of the ability to get federally subsidized health insurance to maintain their coverage.
Cecil also wants providers to help out by reminding their Medicaid patients of their renewal date, which is available on each patient’s KYHealthNet webpage.
For a detailed explanation of the unwinding, see Medicaid’s response to frequently asked questions about member renewals.