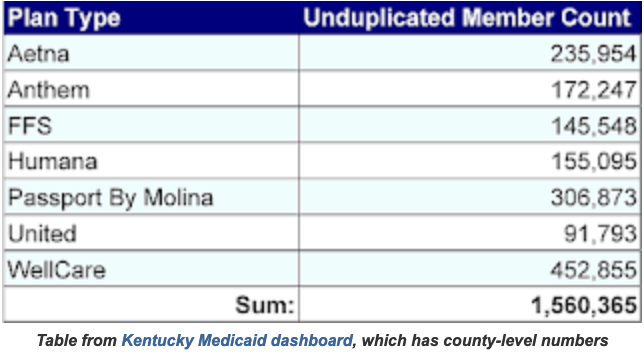
Anthem loses court fight to keep managing Medicaid for 172,000
Kentucky Health News
Anthem Kentucky has failed in its attempt to remain as the manager of Medicaid coverage for about 170,000 Kentuckians, because the Kentucky Supreme Court deadlocked on the insurance company’s appeal of a Court of Appeals ruling that upheld the state’s decision to give the work to five other insurers.
Anthem had questioned the bidding process, and Franklin Circuit Judge Phillip Shepherd ordered rebidding, but some of the other managed-care companies appealed, and in 2022 the state Court of Appeals overturned Shepherd’s decision.
On Anthem’s appeal to the Supreme Court, argued last week, the justices were divided 3-3, meaning that the Court of Appeals decision stands. Justices Angela McCormick Bisig of Louisville, Robert Conley of Ashland and Michelle Keller of Northern Kentucky voted to affirm the appeals court, while Justices Debra Hembree Lambert of Somerset, Christopher Shea Nickell of Paducah and Chief Justice Laurance B. VanMeter of Lexington voted to overturn it.
The seventh justice, Justice Kelly Thompson of Bowling Green, did not hear the case and did not vote. He told Kentucky Health News that he was disqualified because he was involved in the case while on the Court of Appeals.
Anthem had remained a Medicaid manager pending the outcome of the case. The current managed-care contracts expire at the end of 2024, so it will have another chance to get part of the business from the program, which spends $15 billion a year in Kentucky, more than 70 percent of it federal money.